What is Trauma?
Trauma encompasses the enduring effects of distressing events on our brain’s processing, storage, and interpretation of those experiences. In clinical contexts, a singular traumatic incident is commonly known as post-traumatic stress disorder (PTSD), while ongoing traumatic situations like childhood adversity are classified as complex post-traumatic stress disorder (cPTSD). Trauma isn’t solely about the negative events but also the absence of positive ones that should have taken place. As a result, the brain and body develop unique responses to such circumstances. Recent advancements in neuroimaging indicate that trauma’s long-term consequences can impact the brain’s structure, leading to disruptions in mental and physical wellbeing.
Importance of understanding trauma
Understanding trauma is vital, as research demonstrates that adverse childhood experiences (ACEs) can lead to psychological distress in adulthood. Individuals who have faced challenges in childhood may encounter difficulties later in life, such as academic underachievement, limited career progression, relationship issues, and even a shorter lifespan. The renowned ACEs study conducted by Felitti and Anda, which examined over 17,000 adults in the United States, provides some alarming data. The study found over half of the participants had experienced at least one ACE, while one in five had experienced four or more ACEs, and increasing the risk of suicide attempt by 12 times. Furthermore, they concluded that ACEs did not occur in isolation, being subject to one ACE category increased the likelihood of being subjected to other categories by 65-93%. These figures emphasise the need for policies that address the negative effects of trauma in early childhood and its long-term implications.
Understanding the brain and trauma effects
The brain’s response to trauma is of utmost importance, as it can have a profound impact on the individual. Recent advancements in neuroscience have shed light on how trauma can affect the structure and function of the brain. Understanding the effects of trauma on this vital organ is crucial, as the brain is responsible for maintaining overall health and functioning. Specifically, three key regions of the brain are significantly influenced by trauma: the pre-frontal cortex (PFC), the amygdala, and the hippocampus. The PFC acts as the brain’s central processing unit, facilitating logical thinking, risk assessment, and decision-making. The amygdala plays a vital role in regulating emotions and triggering the body’s fight or flight response. On the other hand, the hippocampus is essential for memory formation and storage, organizing and retaining past experiences and reactions.
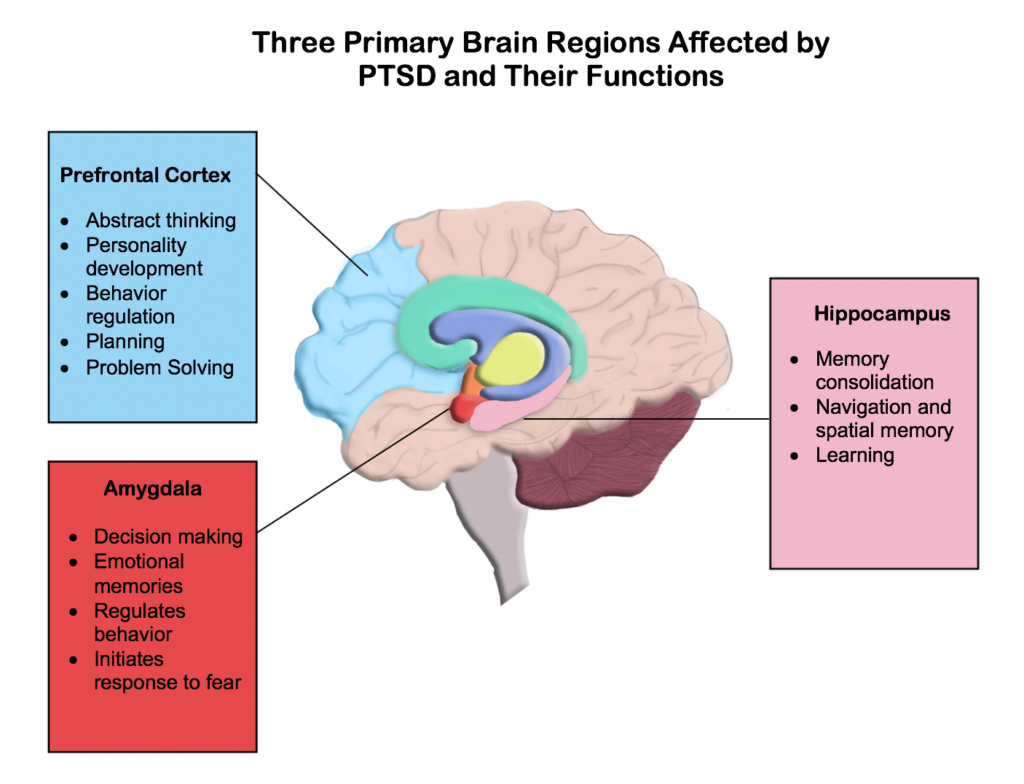
The amygdala acts as the brain’s security system, monitoring emotions and sending messages to other parts of the brain to prepare for potentially dangerous situations. When confronted, the amygdala controls emotional responses and prepares the body for fight or flight reactions. People who have experienced trauma typically have a more active amygdala, making them more sensitive to stress triggers associated with past traumatic experiences. Research suggests that individuals with PTSD often have a smaller amygdala, suggesting a compromised emotional regulation system.
The hippocampus, a brain region linked to learning and memory, can be affected by trauma, altering our stress responses by influencing how past memories are organised. Studies suggest that individuals with cPTSD often have a smaller hippocampus volume, impacting their capacity to differentiate between past and present events. For example, a veteran might instinctively seek cover upon hearing a loud noise resembling gunfire, even in a non-combat setting. This illustrates how the brain can react based on past experiences, even when the current environment is safe.
The prefrontal cortex, located on the outer front side of the brain, is commonly referred to as the brain’s central processor. It plays a crucial role in logical thinking and risk calculations. However, when trauma occurs, it can hinder the functioning of the PFC. The overactive amygdala, which sends signals for emotional responses and releases chemicals, prompts the body to react with fight or flight before the PFC has a chance to assess the balance between threat and safety. As a result, individuals with a history of trauma may exhibit defensive or abrupt reactions when confronted with unexpected challenges. The amygdala takes control, while the hippocampus recalls previously learned responses to danger, overpowering the PFC. Research suggests that individuals with trauma backgrounds may have an underactive PFC.
What can we do to promote healthy brain function?
While the field of neuroscience has provided valuable insights into how trauma affects the brain, research has also highlighted the positive effects of certain interventions in reorganizing our learning patterns and developing adaptive coping mechanisms. These interventions include:
- Cognitive Behavioural Therapy
- Meditation
- Yoga
- Social support and activities